As Covid-19 amplifies existing operational challenges faced by health systems across the country, length of stay management has become especially critical for reducing margin pressure and increasing effective capacity. Many are pursuing strategies to reduce length of stay through more effective discharge planning, in particular beginning discharge planning for patients upon admission. However, in practice, this process is highly variable and difficult to sustain, and there is sparse literature around specific best practices and the true effectiveness of these initiatives.
Best Practices for Reducing Excess Days
New industry-leading research from Qventus uncovers and quantifies best practices for reducing excess days. In analyzing over 75,000 patient visits across hospitals of different sizes, clinical models, and levels of performance, the analysis identified two key drivers.
Best Practice #1: Early discharge planning
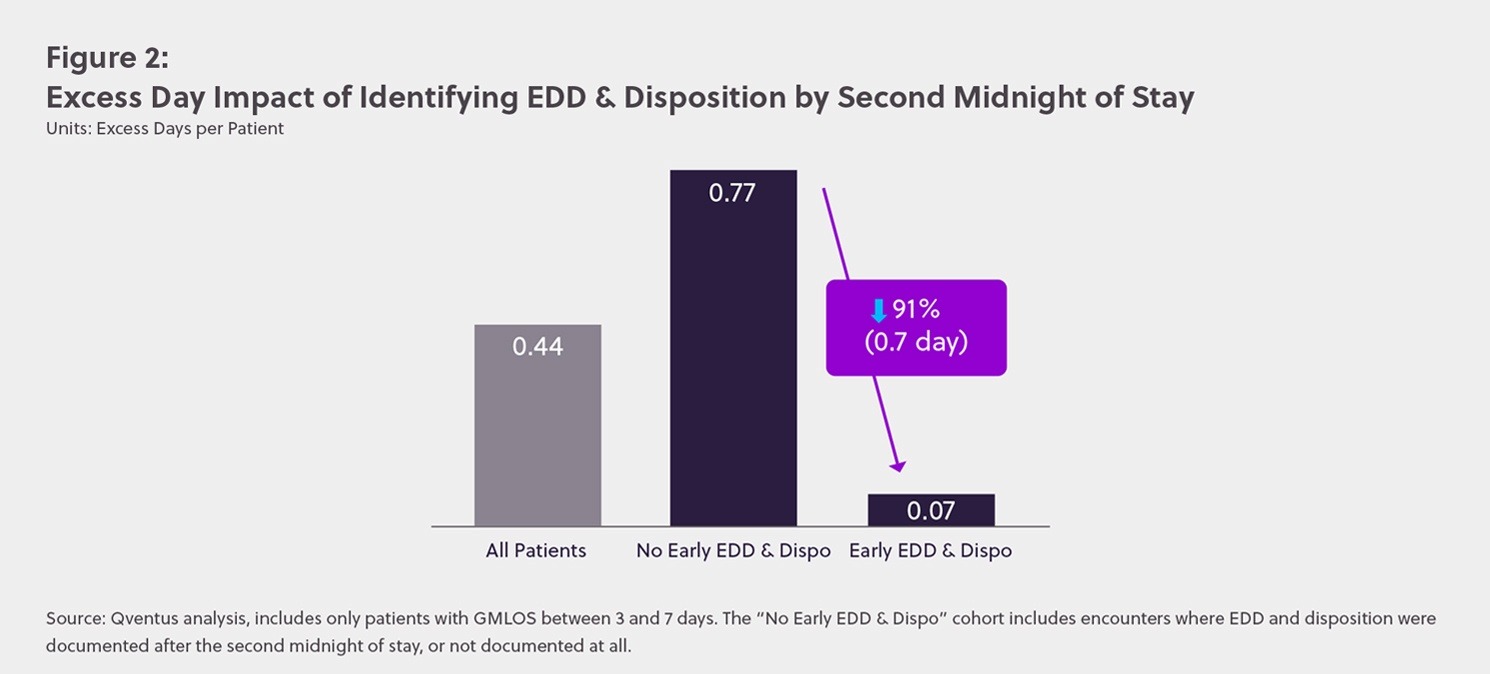
Patients with estimated date of discharge (EDD) and expected disposition identified by the second midnight of stay had 91% fewer excess days.
On average, patient visits analyzed had 0.44 excess days. But the research found a 91% (0.7 day) difference in excess days between patients who had an EDD and expected disposition identified by the second midnight of stay compared to those who did not. This pattern applied across clinical conditions of varying complexities, from sepsis to joint replacements.
Best Practice #2: Proactive barrier management for complex discharges
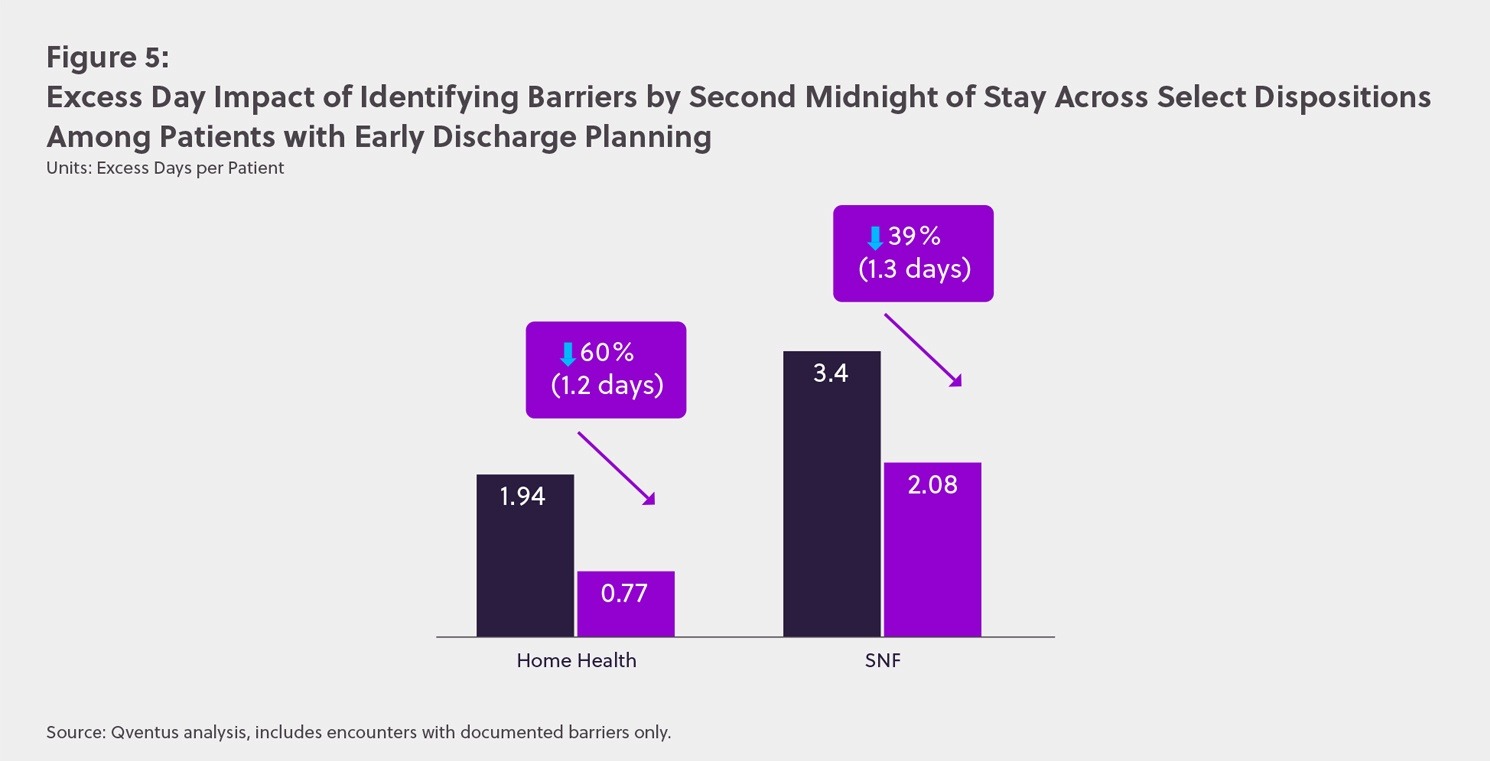
Patients who discharge to SNF or require home health services experienced an excess day reduction of more than 1.2 days when barriers to discharge were identified by the second midnight of stay.
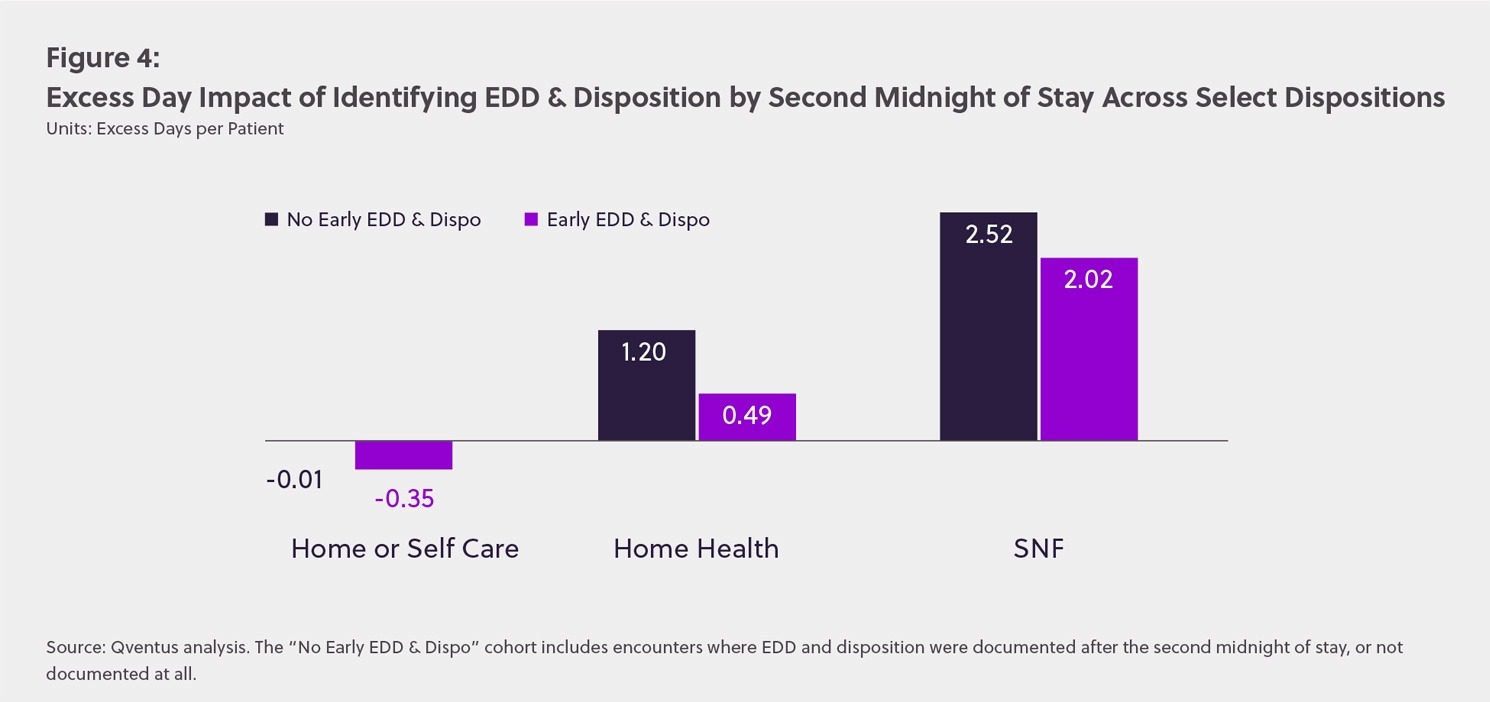
The analysis showed that patients requiring post-acute services or placement continued to drive high levels of excess days, even after accounting for gains achieved by early discharge planning. For example, patients requiring home health services had 0.49 excess days, while those discharging to SNF had 2.02 excess days — even when EDD and disposition were identified before the second midnight of stay. These elevated levels of excess days are not surprising, as care teams need to manage many more process steps and potential bottlenecks (family coordination, therapy services, prior authorization and placement, etc).
For these patients, the research uncovered a second best practice: identifying discharge barriers by the second midnight of stay. For patients requiring home health services, when early discharge planning and barrier identification was conducted, excess days decreased by 60% (1.2 days). For patients discharging to SNF, excess days decreased by 39% (1.3 days) when barriers to discharge were identified early. These findings demonstrate a significant opportunity for care teams to reduce length of stay.
Learn More
Read the full white paper for in-depth analysis around these discharge planning best practices and how progressive health systems are hardwiring processes to drive meaningful reductions in length of stay.


